Engineering a new horizon for persistent depression in the NHS
Commissioning and delivering mental health services is complex – it requires coordination across primary and secondary care, social care and the third sector. With such a complex matrix there’s always a risk of creating silos between pathways and organisations which can be a hurdle when it comes to conducting research and evaluating the impact of commissioning decisions.
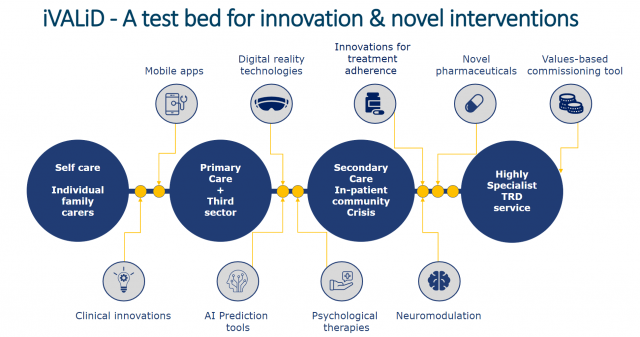
Health Innovation East have partnered with Cambridgeshire and Peterborough NHS Foundation Trust (CPFT), the University of Cambridge and the NIHR Applied Research Collaboration (ARC) for the East of England to develop a values-based approach to the depression pathway, combining patient and clinician perspectives with latest evidence.
This collaborative project, known as informing VALues-based practice in persistent Depression (i-VALiD), was launched in a recent joint conference – Engineering a new horizon for persistent depression in the NHS. We convened health professionals, science and technology partners and experts with lived experience to showcase the latest discoveries that could benefit the services we provide both at CPFT and across the wider NHS system.
Understanding the impact of persistent depression
– 65% of those with depression are in contact with services (mostly in primary care)1
– Lost employment brings the total to £12.2bn2
– 30% of those with depression do not respond to antidepressants2
It was such an inspiring day, so in case you weren’t able to join us, here are four challenges we are aiming to address through the i-VALiD project:
1. Defining values-based practice
When it comes to persistent depression (sometimes referred to as treatment resistant depression), we hope to achieve remission for our patients, prevent relapse and restore physical and social functioning. Values-based practice and commissioning goes beyond quantitative, evidence-based research to use a more qualitative approach. By building upon clinical expertise to include the perspective of people with persistent depression and their carers’, we get a richer idea of the value of an intervention on outcomes and societal impacts over the long-term, especially in individuals suffering multimorbidities.
The i-VALiD project will develop an evidence base rooted in values-based practice which commissioners and providers can draw on when considering the needs of patients with persistent depression in Cambridgeshire and Peterborough and hopefully also across the wider NHS.
2. We need to break down the silos in mental health pathways with a clear purpose
Significant research into the social, biological and psychological processes that cause depression has been conducted over the past 20 years, but as new developments are made, we need to get better at ensuring lessons are applied quickly and consistently across all organisations in contact with service users if we are to get their full benefit.
With the development of Integrated Care Systems we have made great progress at reducing silos within the NHS and the care sector. We need to build on this progress to ensure seamless pathways for people with depression. There are also silos within the research community; an inherent challenge of complex conditions such as depression is that research is sometimes conducted within very different fields which may not always obviously overlap, for example genetics, psychology or gut health. We need to develop a way to bridge these specialties and ensure we gain the full benefit of research across the world.
Finally, we need to tap into the wealth of insight and expertise within the life sciences and innovation community. This includes a robust way of testing what works and supporting adoption consistently across our region whilst stopping interventions shown to be less effective.
We need to bring people together around a unified and clear purpose, drawing on the expertise of organisations like Health Innovation East to convene groups across traditional silos to achieve more together.
3. Better use of data
With the advancement of technology and the digitisation of health information, we can collect data far more effectively to enable us to make the best possible decisions. We will offer all patients on the persistent depression pathway the opportunity to contribute to clinical research, which will allow us to use data to drive change and modify the services we offer across our region.
4. Organising around populations
During our launch event, we heard from Anne Bianchi, who has suffered from persistent depression and shared her experience of attending her local emergency department and the challenges of integrated care across different providers. Personal stories are so powerful at helping us see where services can do more to be joined up and provide a better experience. One size rarely fits all. This is why the values-based approach can be so effective – it is built with a strong patient voice at its core. By listening to the needs of our local population we can develop values-based metrics and identify where in the pathway different interventions may be most effective. We want to empower people in their own care, with treatment measured against their definition of effectiveness.
Why Cambridgeshire and Peterborough?
Our region has all the ingredients we need to be able to bring about changes that could greatly improve the lives of people with treatment resistant depression. With some of the world’s best scientific and clinical expertise, world-class research and an infrastructure to support partnership, we hope that this project will be a catalyst for collaboration. As we learn more, we will build on the i-VALiD project to find themes and challenges where innovation can provide effective solutions and empower clinicians to adopt the interventions they need to help people with depression.
Read two peer-reviewed papers arising from this work:
- Economic evaluation of interventions for treatment-resistant depression: A systematic review
- What outcomes matter to service users who experience persistent depression: A mixed-method narrative review and synthesis
Get involved
Are you interested in partnering with us in the i-VALiD programme to improve the lives of those living with persistent depression though coproduction?
Contact Louise Jopling, PhD, Commercial Director at Health Innovation East at louise.jopling@healthinnovationeast.co.uk

Tracy has more than 30 years’ experience with the NHS in trust and commissioning organisations, including over 15 years at executive level, after beginning her career as a radiographer. She is also a non-executive director at Health Innovation East, the chief executive of Cambridgeshire and Peterborough NHS Foundation Trust and chair of East of England Applied Research Collaborative (ARC). She is also a board member for Cambridge University Health Partners (CUHP) and chair of Cambridgeshire and Peterborough Local People Board and the Eastern NIHR Clinical Research Network.
References
- NICE depression Guidelines 2020
- Treatment-resistant depression: therapeutic trends, challenges, and future directions. Patient Prefer Adherence (Al-Harbi, KS., 2012)
You might also like…

What do we do next to ensure the changes made in primary care work for patients and clinicians?
Read the blog by Dr Simon Rudland (Chair Suffolk GP Federation; Visiting GP Hoy and Walls Practice Orkney; Honorary Senior Lecturer and Digital Health Lead, Norwich Medical School) and Dr Sarah Robinson (Director of Delivery, Health Innovation East).
Share your idea
Do you have a great idea that could deliver meaningful change in the real world?
Get involved
