


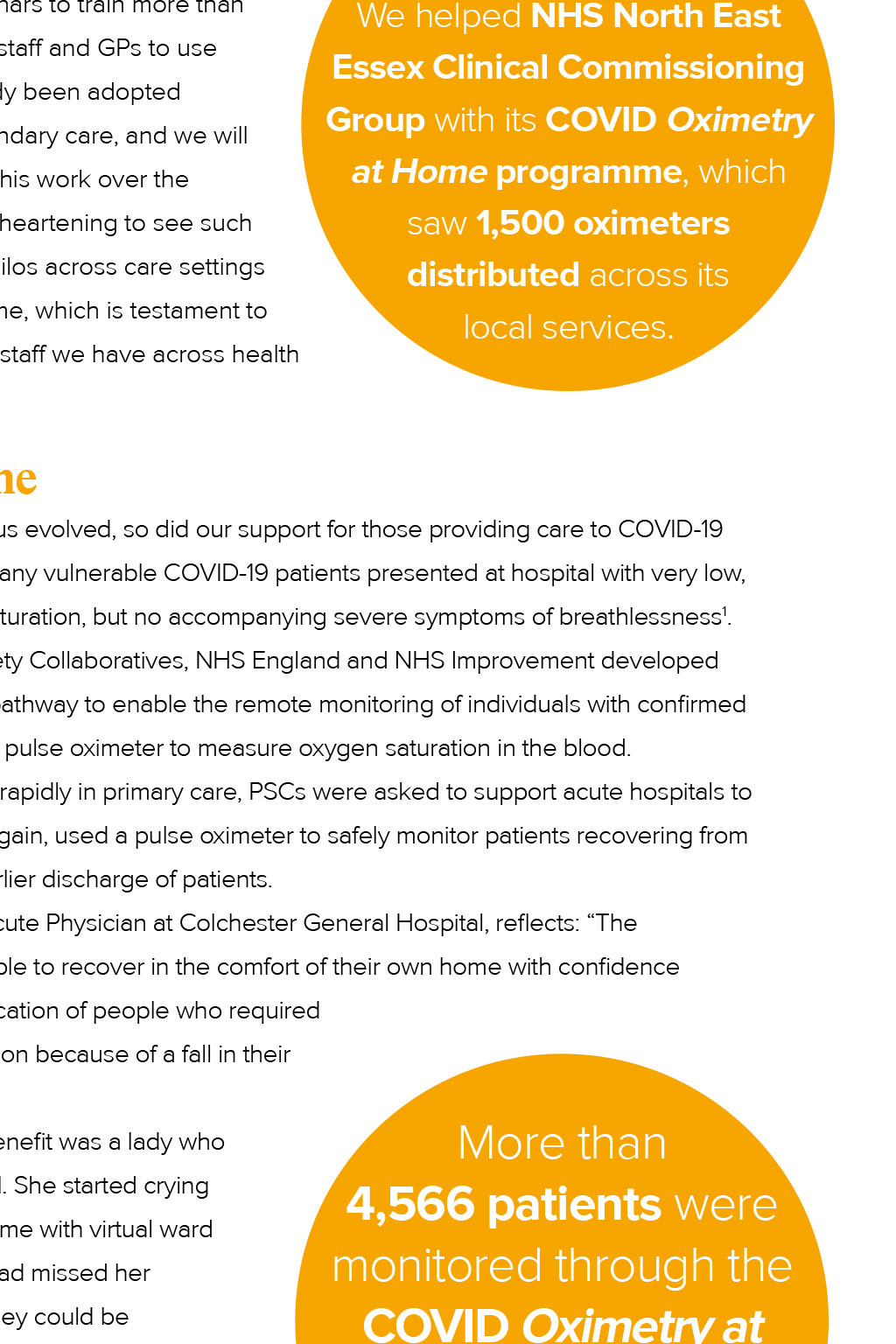






Patient safety Caroline Angel, Director of Patient Safety at Eastern AHSN, highlights the key activities from Eastern AHSNs Patient Safety Collaborative in 2020/21 Click here to Read more about our work rolling out telehealth in our region P atient Safety Collaboratives (PSCs) play an essential role in implementing safer care initiatives across the system, working in acute, non-acute and community settings to quickly share and spread evidence-based practices, products and tools. The PSCs are a joint initiative, funded and coordinated nationally by NHS Improvement and delivered locally by the AHSN Network. and beyond their usual roles in response to the pandemic, including members of our own team, who voluntarily took frontline and logistical roles within the region. Ensuring that the workforce had the right skills and tools to deal with COVID-19 patients was vital. COVID-19 forced healthcare providers to rapidly review almost every activity and piece of equipment within a clinical setting, right down to the layout of wards as increased infection control and social distancing became an immediate priority. This meant that many traditional ways of working were no longer possible, particularly as GPs were restricted from visiting care home residents because of the risk of infection and cross-contamination between patients and sites. Eastern AHSN built on our existing safety improvement programmes to address these challenges Since 2019, we have been working with providers across the East of England to embed tools to better identify and respond to the deterioration of a patients condition (including NEWS2, Soft Signs and SBARD) into local acute and community care settings. We worked with clinical commissioning groups (CCGs) in our scores and escalate them to a clinician using a structured communication tool. We have also included GPs in our training, enabling digital ward rounds and allowing them to deliver care Did you know? remotely. We were able to use webinars to train more than the system, which has already been adopted across ambulance and secondary care, and we will This animation will inform you about COVID-19, how to measure your oxygen levels (using a pulse oximeter), what the danger signs to look out for are and when to seek urgent help. be evaluating the impact of this work over the summer. Its been incredibly heartening to see such progress in breaking down silos across care settings during such a challenging time, which is testament to We helped NHS North East Essex Clinical Commissioning Group with its COVID Oximetry programme, which 1,500 oximeters distributed across its local services. and social care. What is NEWS2 and SBARD? Oximetry at Home As our understanding of the virus evolved, so did our support for those providing care to COVID-19 NEWS2 National Early Warning Score 2: a standardised tool used to identify and escalate a deteriorating patient, by measuring a set of key physiological parameters. and sometimes fatal, oxygen saturation, but no accompanying severe symptoms of breathlessness1. To address this, the Patient Safety Collaboratives, NHS England and NHS Improvement developed the COVID Oximetry at Home or suspected COVID-19 using a pulse oximeter to measure oxygen saturation in the blood. As the programme rolled out rapidly in primary care, PSCs were asked to support acute hospitals to implement virtual wards. This, again, used a pulse oximeter to safely monitor patients recovering from SBARD Situation, Background, Assessment, Recommendation and Decision: a framework to guide structured communication of a patients condition when COVID-19 at home or in care homes, allowing earlier discharge of patients. further assessment and admission because of a fall in their blood-oxygen level. member to another. had spent eight days in hospital. She started crying We supported primary and secondary care colleagues to rapidly implement the service, being a critical friend to systems and sharing good practice and learning from across the country. We hosted a series of webinars and training sessions to support More than 4,566 patients were monitored through the COVID Oximetry at Home pathway from 1 Nov 2020 to 28 Feb 2021 the rapid uptake of the Oximetry at Home and virtual ward models. By the end of March 2021, the programme was successfully rolled out across all our CCGs and all but one acute trust in the Eastern region. Dr Melanie Iles, Medical Director, System Improvement and Professional Leadership (East of England) at NHS England and NHS Improvement: Ensuring safe tracheostomy care Eastern AHSNs PSC worked with the National Tracheostomy Safety Project (NTSP) to embed elements of a toolkit to support healthcare A tracheostomy is an opening created at the front of the neck so a tube can be inserted into the windpipe (trachea) to help you breathe. The COVID-19 pandemic saw a sharp rise in patients requiring relatively prolonged ventilatory support, many of whom have required temporary tracheostomies and were often not cared for in permanent, established intensive care unit settings. The toolkit gives information, practical resources and links to useful skills and knowledge to appropriately care for these patients. Working individually with the acute hospitals in the region, we supported the tracheostomy care leads and critical care training lead nurses Richardson S, Hirsch J S, Narasimhan M, et al. (2021). Remote management of COVID-19 using home pulse oximetry and virtual ward support. BMJ. 372:n677 1 References to rapidly review the toolkit against current policies, with all adoption of the three safety interventions. This was a priority Improving maternity care Part of the Maternity and Neonatal Safety Improvement Programme, the Preventing Cerebral Palsy in Pre-term Labour (PReCePT) programme aims to ensure mothers going into labour before 30 weeks are sulphate, which costs just 1 and reduces the risk of cerebral palsy. Despite the pandemic, we worked with all 11 maternity units across the region to successfully maintain the excellent 86% rate achieved last year. high volumes of patients requiring a tracheostomy. If you are interested in patient safety in our region and would like to get in touch, contact Caroline at caroline.angel@eahsn.org Share this article Learning from experience Care during a crisis: Learning from the military-style NHS response to COVID-19 Tania Holland, Quality Improvement Project Manager Four things I learned working on the intensive care ward during COVID-19 Tara Marshall, Clinical Lead for Deterioration