

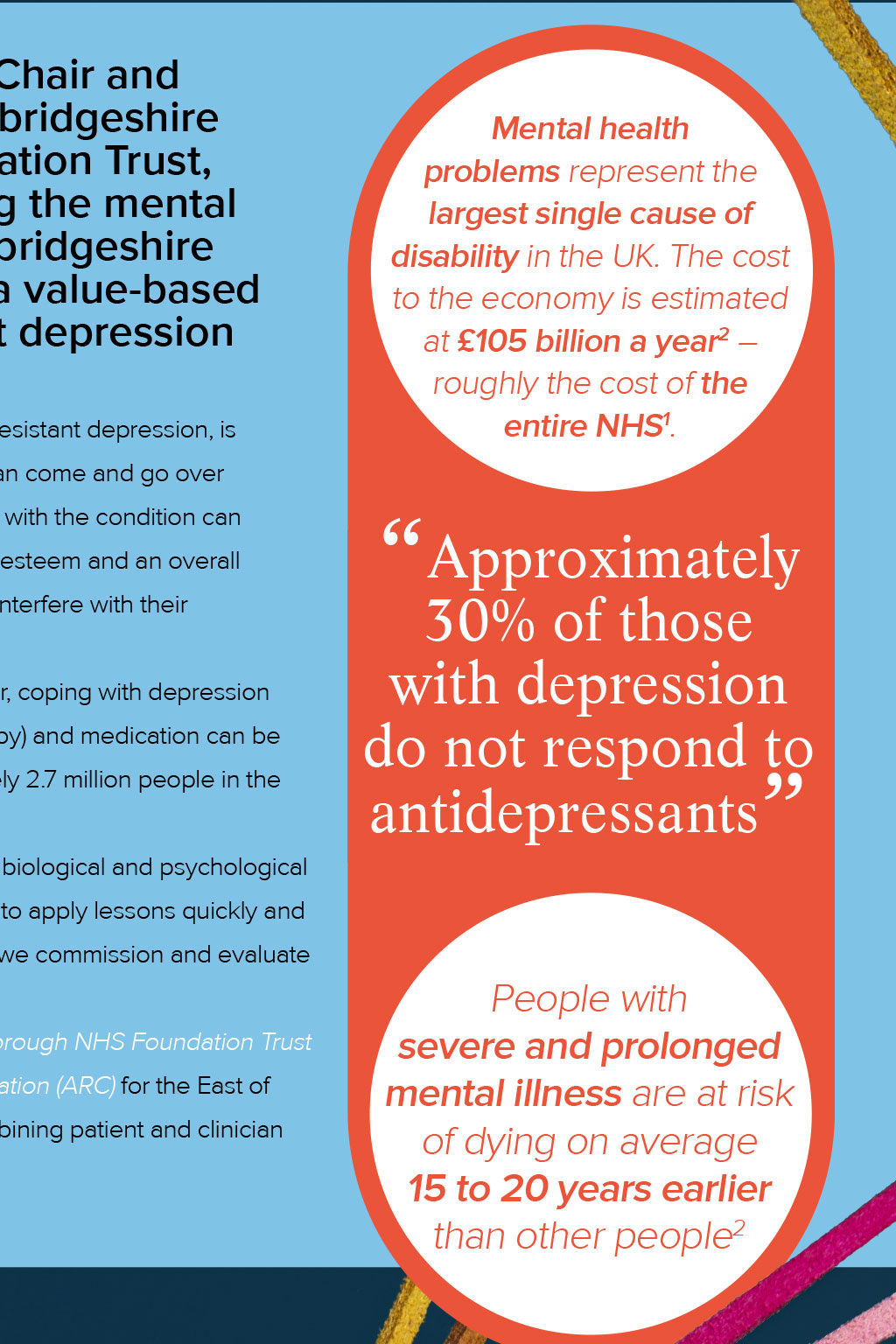
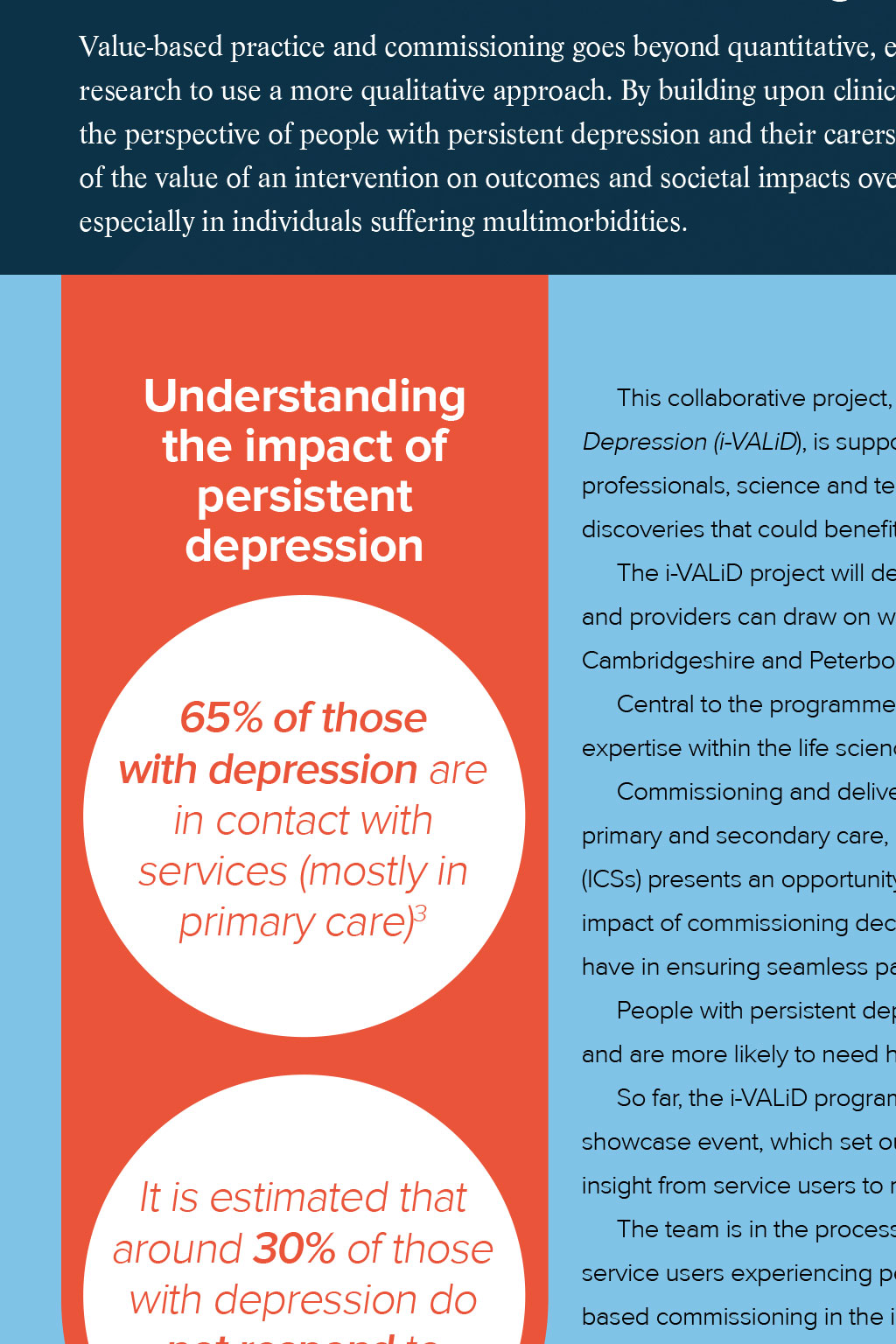



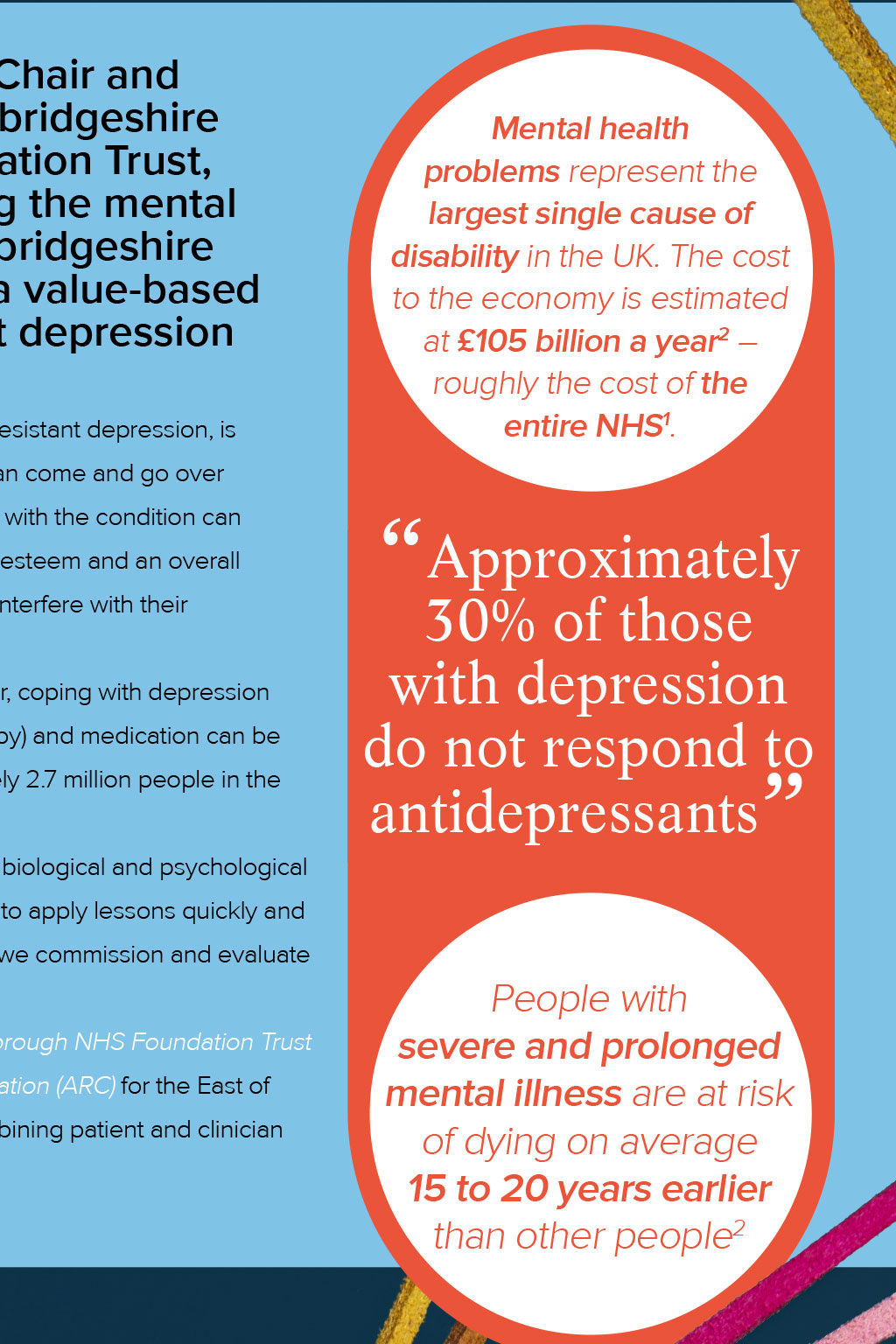
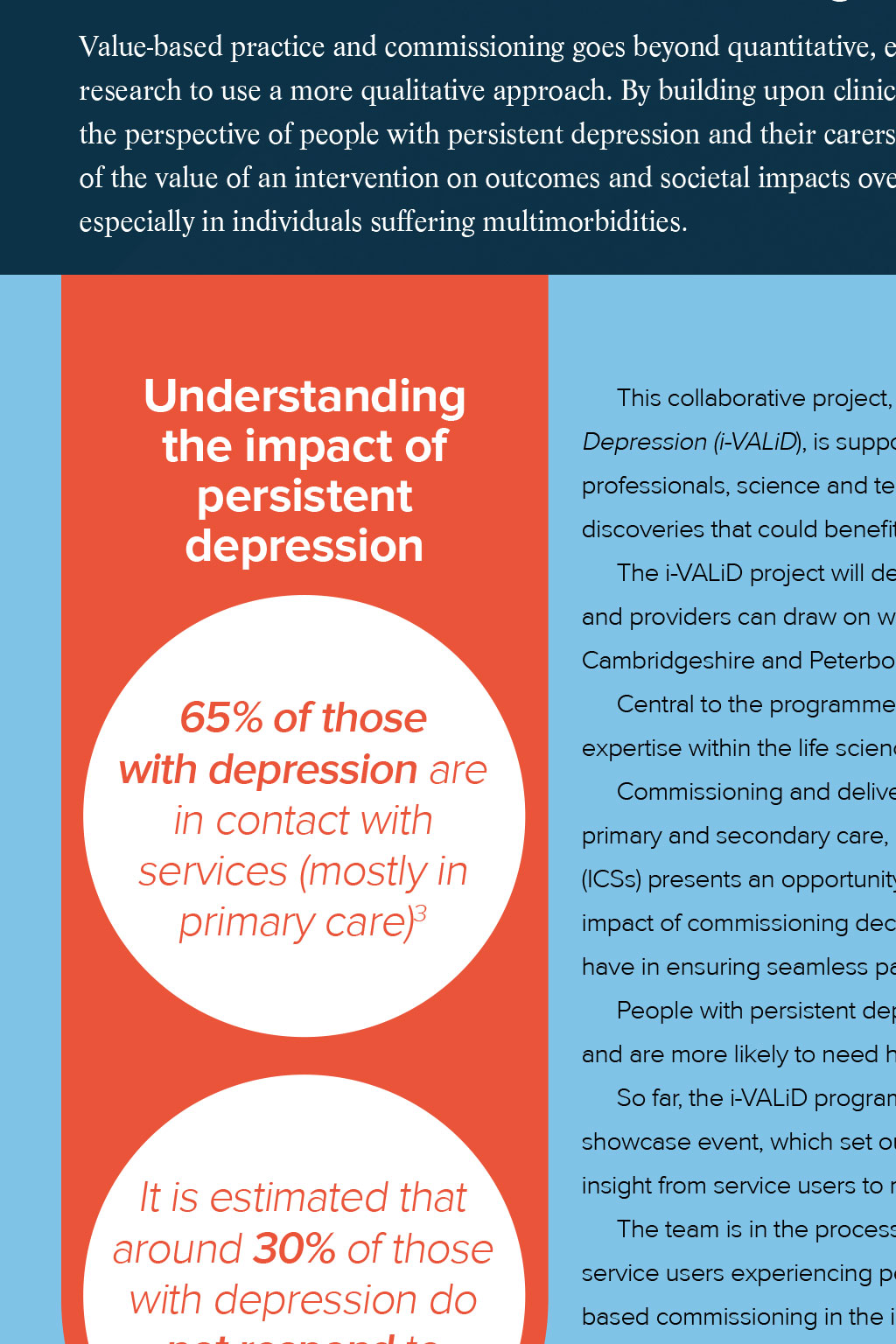

Mental health Tackling depression treatment-resistant Tracy Dowling, Eastern AHSN Chair and former Chief Executive of Cambridgeshire and Peterborough NHS Foundation Trust, explains how we are convening the mental health community across Cambridgeshire and Peterborough to develop a value-based approach to treating persistent depression P Mental health problems represent the largest single cause of disability in the UK. The cost to the economy is estimated at 105 billion a year2 roughly the cost of the entire NHS1. ersistent depressive disorder, also called dysthymia or treatment-resistant depression, is a continuous long-term form of depression, although symptoms can come and go over a period of years and their intensity can change over time. People with the condition can lose interest in normal daily activities, feel hopeless, have low self-esteem and an overall feeling of inadequacy. These feelings can last for years and may significantly interfere with their relationships, school, work and daily activities. Because of the long-term (chronic) nature of persistent depressive disorder, coping with depression symptoms can be challenging. A combination of talking therapy (psychotherapy) and medication can be effective. However, approximately 30% of those with depression (approximately 2.7 million people in the UK1) do not respond to antidepressants. Approximately 30% of those with depression do not respond to antidepressants Over the past 20 years there has been significant research into the social, biological and psychological processes that cause depression. As new developments are made, we need to apply lessons quickly and consistently across mental health services and ensure that the ways in which we commission and evaluate services, models of care and innovations are as effective as possible. Thats why Eastern AHSN has partnered with Cambridgeshire and Peterborough NHS Foundation Trust (CPFT), the University of Cambridge and the NIHR Applied Research Collaboration (ARC) for the East of England to develop a value-based approach to the depression pathway, combining patient and clinician perspectives with latest evidence. People with severe and prolonged mental illness are at risk of dying on average 15 to 20 years earlier 2 than other people What is value-based commissioning? Value-based practice and commissioning goes beyond quantitative, evidence-based research to use a more qualitative approach. By building upon clinical expertise to include the perspective of people with persistent depression and their carers, we get a richer idea of the value of an intervention on outcomes and societal impacts over the long term, especially in individuals suffering multimorbidities. Understanding the impact of persistent depression This collaborative project, known as informing VALues-based practice in persistent Depression (i-VALiD), is supported by a Medical Education Grant from Janssen and has convened health professionals, science and technology partners, and experts with lived experience to showcase the latest discoveries that could benefit the services we provide, both at CPFT and across the wider NHS system. The i-VALiD project will develop an evidence base rooted in value-based practice that commissioners and providers can draw on when considering the needs of patients with persistent depression in Cambridgeshire and Peterborough and, hopefully, also across the wider NHS. 65% of those with depression are in contact with services (mostly in 3 primary care) Central to the programme is patient input, better use of data and tapping into the wealth of insight and expertise within the life sciences and innovation community. Commissioning and delivering mental health services is complex and requires coordination across primary and secondary care, social care and the third sector. The establishment of integrated care systems (ICSs) presents an opportunity to break down silos and rethink how we conduct research and evaluate the impact of commissioning decisions, so were really excited to see the impact the i-VALiD programme can have in ensuring seamless pathways for people with depression. People with persistent depression have a poorer quality of life, are more likely to need time off work and are more likely to need hospital treatment than those with other forms of depression5. So far, the i-VALiD programme has convened experts across the health and care spectrum at our showcase event, which set out the ambition and capabilities of the project, and we are currently gathering It is estimated that around 30% of those with depression do not respond to 4 antidepressants insight from service users to map the care pathway and identify any potential gaps that could affect care. The team is in the process of publishing a peer-reviewed evaluation of the outcomes that matter to service users experiencing persistent depression and how these are measured (or could be) to aid valuebased commissioning in the implementation of specialist services. We will also be publishing a systematic review of the health economic measures that are utilised within mental health, and particularly depression, to ensure that we are accurately incorporating the wider societal impacts of depression. The findings from these publications will inform future service design for value-based commissioning and we continue to collaborate with researchers and industry partners to maximise the impact of our services for patients and service providers. Improving patient safety in mental health services The Mental Health Safety Improvement Programme aims to improve the safety and outcomes of mental health care by reducing unwarranted variation and providing a high-quality healthcare experience. The programme is designed to support teams to deliver safer services for all, using a systematic approach to how they improve. Share this article Return to the contents page This is a national patient safety improvement programme being delivered in our region by the Eastern Patient Safety Collaborative (PSC), which is funded and nationally coordinated by NHS England and NHS Improvement, and hosted locally by the Academic Health Science Networks (AHSNs). Find out more here. Are you interested in partnering with us in the i-VALiD programme to improve the lives of those living with persistent depression though coproduction? Contact Louise Jopling, PhD, Commercial Director at Eastern AHSN at louise.jopling@eahsn.org Up next: Our impact in numbers References McLachlan G. (2018) Treatment-resistant depression: what are the options? BMJ. 363 :k5354 doi:10.1136/bmj.k5354 2 NHS England. (2016). Five Year Forward View for Mental Health. Available: https://www.england.nhs.uk/wp-content/uploads/2016/02/Mental-Health-Taskforce-FYFV-final. pdf. Last accessed 25/04/22. 3 NICE. (2009). Depression: the treatment and management of depression in adults. Available: https://www.nice.org.uk/guidance/cg90/documents/depression-in-adultsupdate-full-guideline-prepublication2. Last accessed 25/04/22. 4 Al-Harbi, K.S. (2012). Treatment-resistant depression: therapeutic trends, challenges, and future directions. Patient Prefer Adherence. 6, 369388. 5 Jaffe, D., Rive, B and Denee, T.R. (2019). The humanistic and economic burden of treatment-resistant depression in Europe: a cross-sectional study. Available: https:// bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-019-2222-4. Last accessed 25/04/22. 1